OSTEOPOROSIS
Osteoporosis is a global problem, which is increasing in significance as the population of the world both grows and ages. For these reasons, osteoporosis is often referred to as the "silent epidemic." (or)
Osteoporosis is a silent disease of progressive bone loss associated with an increased risk of fractures. It literally means "porous bone." Osteoporosis often causes a loss of height and dowager's hump (a severely rounded upper back).
1. CAUSES OF OSTEOPOROSIS
2. SIGNS OF OSTEOPOROSIS
3. DIAGNOSIS OF OSTEOPOROSIS
4. PREVENTION OF OSTEOPOROSIS
5. TREATMENT OF OSTEOPOROSIS
Osteoporosis is characterized by a decrease in bone mass and density, that leaves porous spaces (holes) in the bones.
This causes a loss of the supporting mineral bone structure, weight and height loss, thin, painful, brittle bones, and easily broken bones. In women, the rate of bone loss speeds up during menopause, a time when levels of the hormone estrogen fall. Bone loss may also occur if both ovaries are removed by surgery.
“World osteoporosis day”- October 20
THE SKELETON
The skeleton is made up of over 200 bones. It is a rigid framework which gives shape and support to the body.
Bone is a highly vascular (large blood supply), living, constantly changing, mineralized connective tissue. The organic matrix (structure) of bone is made up of bone salts, which give bones their hardness and rigidity.
The most important of these bone salts are: calcium, magnesium, phosphate, carbonate, hydroxyl, chloride, fluoride (elemental), and citrate.
1. CAUSES OF OSTEOPOROSIS
Top
-
Mineral (calcium and magnesium) deficiencies
-
A lack of estrogen
-
Early menopause (before age 45)
-
Early hysterectomy (before the age of 45), particularly when both ovaries are removed (oophorectomy)
-
Missing periods for six months or more (excluding pregnancy) as a result of over-exercising or over-dieting.
-
Long-term use of high dose corticosteroid tablets (for conditions such as arthritis and asthma)

-
Close family history of osteoporosis (mother or father)
-
Other medical conditions such as Cushing's syndrome and liver and thyroid problems
-
Malabsorption problems (Celiac disease, Crohn's disease, gastric surgery)
-
Long-term immobility
-
Smoking

-
Heavy metal and environmental chemical exposure (especially cadmium and nickel) are all underlying factors of osteoporosis.
-
Excessive consumption of animal protein, sugar, salt, caffeine, soft drinks and heavy drinking
There are many misconceptions about osteoporosis, for example that it is "an old woman's disease." The lifetime risk for a woman to have an osteoporotic fracture is 30-40%. In men, the risk is about 13%.
2.SIGNS OF OSTEOPOROSIS
Top
Signs include a broken wrist or hip, low back pain or a hunched back. This is because osteoporosis can cause the bones in spine (called the vertebrae) to collapse. This is called compression fracture and can cause severe back pain. These problems can occur after a lot of bone calcium has been lost.
3. DIAGNOSIS OF OSTEOPOROSIS
Top
Bone densitometry is a safe, painless X-ray technique that compares bone density to the peak bone density that someone of same sex and ethnicity should have reached at about age 20 to 25.
Dual beam X-ray absorptiometry (DXA) is one of the most accurate methods, but other techniques can also identify osteoporosis, including single photon absorptiometry (SPA), quantitative computed tomography (QCT), radiographic absorptiometry and ultrasound.

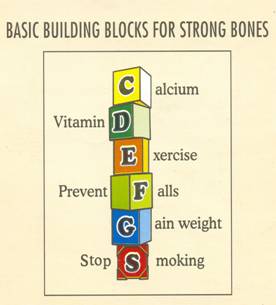
4. PREVENTION OF OSTEOPOROSIS
Top
Osteoporosis is a very preventable disease. Building strong bones in childhood and adolescence is the best defense.
-
Maintain a calcium rich diet (1,000 to 1,500 mg/ day)
-
Get plenty of Vitamin D
(400 and 800 IU / day)
-
Engage in weight bearing exercises.
-
Consider hormone replacement or other medications if at risk.
5.TREATMENT OF OSTEOPOROSIS
Top
Exercise and nutrition therapy are often key components of a treatment plan for osteoporosis and there are other treatments as well. Estrogen replacement therapy (ERT) is often recommended for women at high risk for osteoporosis to prevent bone loss and reduce fracture risk.
According to Indian Council of Medical Research, the calcium intake/ day for each individual are
Males, females (Sedentary, moderate, heavy) |
- |
400mg/day |
Pregnant and lactating women |
- |
1000mg/day |
Women after menopause |
- |
1000-1500mg/ day |
CALCIUM RICH FOODS/ FOODS TO BE INCLUDED
| Cereals |
Ragi (malted) |
| Pulses |
 Soya bean, Rajmah, bengalgram Soya bean, Rajmah, bengalgram
(whole) |
| Green leafy vegetables |
 Agathi, Amaranthus sp (Mulla keerai, Arai keerai, Kuppa keerai), Chekkur manis, Curry leaves, Drumstick leaves, Kuppa meni, Agathi, Amaranthus sp (Mulla keerai, Arai keerai, Kuppa keerai), Chekkur manis, Curry leaves, Drumstick leaves, Kuppa meni, |
| Roots and tubers |
Carrot, tapioca/yam, Sweet potato |
| Other vegetables |
Sundakai dry, ladies finger, drumstick, and lotus stem dry |
| Fruits |
Dates dry, raisins, lime, wood apple, amla |
| Fishes and other sea foods |
 Boal (Valai), Crab (Nandu), Jew fish (Vella Keluthi), Mackerel (Kana keluthi), Parsey dried (Chirayakandai), Shrimp dried Boal (Valai), Crab (Nandu), Jew fish (Vella Keluthi), Mackerel (Kana keluthi), Parsey dried (Chirayakandai), Shrimp dried |
| Milk and milk products |
 Milk (buffalo), Skimmed milk powder, curd, Yoghurt, cheese Milk (buffalo), Skimmed milk powder, curd, Yoghurt, cheese |
FOODS TO BE AVOIDED: Sugar, Refined grain and flour, caffeine (Coffee, tea, cocoa beverage, chocolate), alcohol.
Calcium content in some common Indian foods (mg/100g)
Ragi (malted) |
334 |
Soya bean |
240 |
Bengal gram (whole) |
202 |
Sundakai dry |
390 |
Agathi |
1130 |
Drumstick leaves |
440 |
Mulla keerai |
800 |
Arai keerai |
364 |
Milk (buffalo) |
210 |
|

